Best Radiologist in India
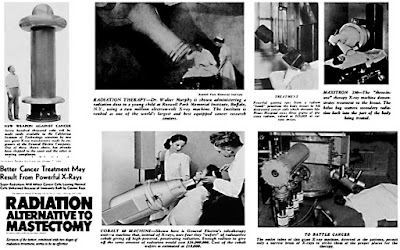
An Introduction to
Radio Therapy
•
Radiation
Oncology syn: RadioTherapy, is a
branch of medicine that utilizes Ionizing Radiation of various types
& energies to treat cancer &
some benign conditions.
•
With rapid technological advancements, the
precision and accuracy has evolved rapidly to make RadioTherapy
indispensable in the multi-modality management of cancer
•
The propagation/transmission of energy from a
Radiative Source to another medium is termed Radiation.
•
Transmission of energy can be in the form of
Electromagnetic waves or Particulate Radiation.
•
Ionizing (High Energy)
•
Non-Ionizing (Low Energy)
1. Radio
waves
2. Microwaves
3. Infrared
4. Visible
Light
5. Ultraviolet
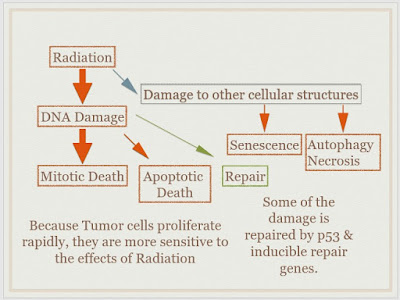
Cellular
effects of Radiation
•
Ionizing Radiation injects energy into a
material, like a microscopic bullet, until the radiation is stopped by the
material due to absorption.
•
On the cellular level, Radiation damages all molecules
of the cell, but the ultimate target is the DNA, which will eventually kill the
cell.
•
Repair (of Sublethal Damage)
·
Sublethal Radiation induced damage is repaired
& helps Tumor cells (and normal tissue) recover.
•
Repopulation
·
Both Tumor cells & Normal tissue cells
proliferate & mitigate the effect of RT
•
Reoxygenation
·
Hypoxic cells are resistant to radiation.
·
Since a major part of the tumor is hypoxic,
reductions in size after a fraction of Radiotherapy reoxygenates previously
hypoxic cells, making them radiosensitive.
•
Reassortment
·
Dividing cells are sensitive to RT in specific
phases of the cell cycle
·
As tumor cells are in different phases of the
cell cycle, those in radiosensitive phase get killed first. Remaining cells
continue the cycle and are killed at the next fraction of RT when they reach
Radiosensitive phase.
•
According to AIM
1.
Curative syn.
Definitive RT: Application of RT ALONE to achieve cure. e.g. Early Head & Neck, Early Cervix
2.
Palliative RT: Application
of RT to alleviate symptoms of Cancer. e.g. Bone metastases, Brain Metastases,
Superior Vena Cava Obstruction
3.
Prophylactic: Application
of RT to prevent relapse in relapse-prone areas. e.g. Prophylactic Cranial
Irradiation in Leukemias
•
According to TIMING & combination with
other modalities
1.
Adjuvant RT: Application
of RT after any kind of treatment modality. If given immediately after
surgery, post-op RT
2.
Neo-Adjuvant RT: Application
of RT before any kind of treatment modality. If given immediately before
surgery, pre-op RT
3.
RadioChemotherapy syn. Concurrent
ChemoRadiotherapy (CCRT): Application of RT concurrently with
Chemotherapy. Can be Adjuvant or Neo-Adjuvant.
•
According to MODE of delivery of
Radiotherapy
•
External Beam RadioTherapy: Given
externally to the patient by a treatment machine e.g. Linear Accelerator
•
Brachytherapy: Given
by implanting Radioactive sources directly on patient (Interstitial) or
in body cavities (Intracavitary).
•
Intra-Operative RadioTherapy: Given
directly to Tumor Bed at time of surgery.
•
Stereotactic Radiotherapy/RadioSurgery: Given
externally by utilizing a rigid frame to deliver high doses in few fractions,
to critical sites (e.g. CNS tumors) using a special machine. e.g. Gammaknife
•
According to PRECISION
•
2 Dimensional (Traditional) Radiotherapy: Obsolete.
Minimal sparing of normal tissue
•
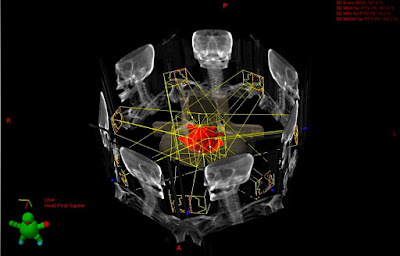
3
Dimensional Conformal Radiotherapy (3D-CRT): RT
delivered by conforming Radiation dose around tumor. Spares some normal
tissue
•
Intensity Modulated Radiotherapy (IMRT): A
Highly developed form of 3DCRT, in which the radiation dose is tightly
conformed around tumor. Spares most normal tissue.
•
Image Guided Radiotherapy (IGRT): IMRT
delivered in conjunction with a daily CT scan of patient done by the treatment
machine. Used to account for changes in size of tumor and accurately adjust for
variations in normal tissues.
•
Spatial Co-operation - 'The Steel Paradigm'
•
Scenario where full strength CT & RT act
independently, with Non-overlapping Toxicity Profiles
•
Ideally, RT (Local Control) + CT (Systemic
Control) = Improved outcomes
•
Few CT agents meet this criteria due to -
Limited Single agent activity + Toxicity driven dose reductions
•
In Field Co-operation
•
Scenario where CT & RT act together to
increase Tumor cell kill.
•
Full Dose RT (Local Control) + Reduced Dose CT
(Enhances RT effect + Cytotoxic Effect) = Improved outcomes
•
Strictly, Radiosensitizer - Enhances RT effect
ONLY (e.g. Misonidazole)
•
Low Dose CT - Radiosensitizer + Cytotoxic
effect
•
If Antagonistic action, then Radioprotective
•
Recommended for all WHO Grade II/III/IV tumors.
•
Nasal Cavity + ParaNasal Sinus: Adjuvant RT for
close/positive margins, PeriNeural Invasion (PNS - Adenoid Cystic Histology).
Adjuvant CCRT for Lymph Node +ve
•
Oral Cavity Cancers - Adjuvant RT for Close
Margins, Stage III/IV, Lymphovascular/ PeriNeural Invasion +ve, Oral Cavity Ca
with Level IV/V Lymph Node +ve. Adjuvant CCRT for Margins +ve, Extracapsular
spread +ve.
•
Oropharynx, Larynx, Hypopharynx - Upfront
surgery not preferred. If performed, Indications remain the same as for Oral
Cavity Ca. Additional Indications for Adjuvant RT - pN2-N3, Cartilage Invasion
(+ Greater than 1 cm subglottic invasion - Larynx only)
•
Salivary Glands - Adjuvant RT for Close/
positive margins, Intermediate-High Grade, Adenoid Cystic Histology, LVI/ PNI,
T3-T4, LN +ve
•
Medullary Carcinoma Thyroid: Adjuvant RT for
Positive margins, Extensive LN +ve, T4a.
•
NSCLC - Resectable stage I/II: Adjuvant RT for
Close (<5 mm)/ Positive Margins.
•
GI Cancers
1.
Esophagus: Resectable Node -ve (Non-Cervical).
Unfavorable T2N0, T3/T4, N+ve or Close/Positive margins - Adjuvant CCRT (RT +
Cisplatin/5-FU)
2.
Stomach: Resectable Node +/ -ve. Adjuvant CCRT
(Mc Donald's - RT + Leucovorin/5-FU).
3.
Pancreas: Resectable. Adjuvant treatment
controversial. Adjuvant Chemo (Gemcitabine) followed by CCRT (RT + 5-FU) -
suggested
4.
GB: Resectable T1b or advanced. Adjuvant CCRT
(RT + 5-FU)
5.
Biliary Tract (Intra/ Extra - hepatic):
Resectable with Residual disease. Adjuvant CCRT (RT + 5-FU - Stereotactic RT
preferred)
6.
Colo-Rectal: Resectable Stage I - Adjuvant CCRT
for T2(RT + 5-FU). Stage II/III - Chemo(5-FU) followed by CCRT(RT + 5-FU)
followed by Chemo(5-FU) vs NeoAdjuvant CCRT (RT + 5-FU) followed by surgery
followed by Chemo (5-FU)
7.
Anal: Resectable T1-T2, Node -, Close or
positive margins. Adjuvant CCRT (RT + 5-FU/ Mitomycin)
•
Breast - RT
is an integral part of Breast Conserving Treatment (BCT). Even patients
undergoing Mastectomy need Post Mastectomy RT (PMRT).
•
In situ disease: BCT for DCIS
•
Early Stage (I-IIB +/- T3N0): BCT vs Total
Mastectomy + PMRT for T3/T4, positive margins, extracapsular spread and 4 or
more Axillary nodes.
·
For T1-T2, 1-3 Axillary nodes: Consider PMRT
for 20% or more positive nodes, size, margins, LVI, Age, Grade
·
For T1-T2, N0: Consider PMRT for Close/positive
margin, Age, LVI, Grade
•
Locally advanced: Chemo followed by Surgery.
Mastectomy or BCT
• Genitourinary Cancers
•
Bladder - Non Muscle Invasive: Adjuvant RT for
Abnormal Cytology, Multifocal Disease, High Grade histology, Subtotal Resection
•
Prostate - Adjuvant RT for Margins +, Residual
disease on Imaging/Biopsy or pT3 disease
•
Urethral - NeoAdjuvant RT for Distal Lesions or
Lesions involving the entire urethra
•
Testicular - Seminoma (Limited to Testis):
Adjuvant RT
•
Penis - Organ Preservation Approach -
Increasingly favored based on Anal & Vulvar Ca results. Adjuvant RT for
Node +
The indications for Definitive Radiotherapy/CCRT are numerous and continue to increase
with ongoing Research.
Palliative Radiotherapy is an effective method of controlling
some of the most distressing symptoms due to metastatic disease (irrespective
of Primary).
Call us for More Details: +91 9811996326
E-mail: admin@radiotherapy.in
Visit: oncocare.in










No comments:
Post a Comment